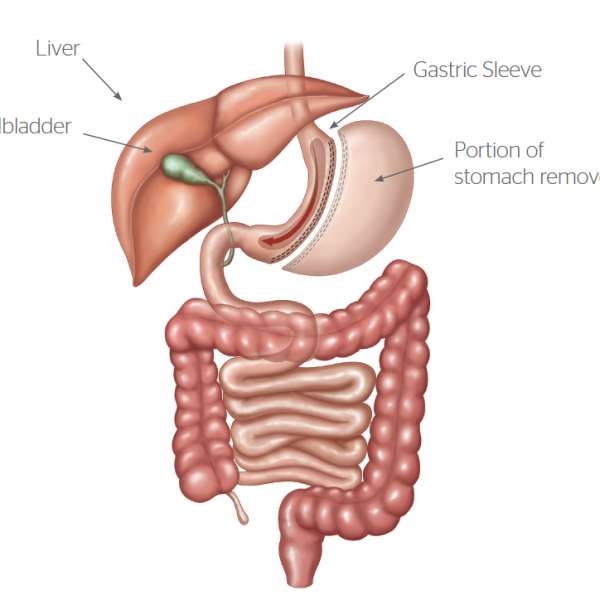
What is Sleeve Gastrectomy?
The sleeve gastrectomy (SG) is a restrictive weight loss operation. The outside part of the stomach is removed and the shape of the stomach is changed from a sac to a long narrow tube. The gastric volume is reduced from approximately 2 Liters to 100 mL. Furthermore the outside part of the stomach which produces the hunger hormone Grehlin is removed, resulting in an initial profound loss of appetite. This effect tends to lessen with time, but nevertheless long term, there is less hunger.
The main effect of the SG is thought to be the reduced volume of food needed to feel full and satisfied. Using the SG as a tool for portion control allows the committed patient to eat 3 small meals per day and feel satisfied, unlike being on a diet. The subsequent reduction in caloric intake will result in weight loss. Good food choices as well as regular exercise are also necessary to optimise outcome.
Advantages of Sleeve Gastrectomy
The advantage of SG over the other restrictive operations such as the gastric stapling operation (VBG) or the adjustable band (AGB) is that with the SG the whole gastric tube fills when eating so patients feel full rather than obstructed. As the SG does not have a band, there are not many food intolerances in the long term. Bread, meat and fruits can be consumed albeit at a reduced volume and speed. Therefore it allows for eating a healthy balanced diet. If an operation does not allow people to eat a healthy diet then long-term outcomes will be difficult and potentially jeopardized.
Success with weight control is characterized by 3 small meals per day of lean source protein, low starch carbohydrate, adequate fruits and vegetables and aiming to keep caloric intake low (Daily: less than 1300 Kcal for women and less than 1500 Kcal for men). The SG with reduced hunger and early satiety (fullness) gives people a powerful tool to comply with the low calorie meals plan long term. It is unlike being on a diet.
In summary the main advantages of the SG over AGB are less obstructive eating, more rapid weight loss, no foreign body, no adjustments, and greater end weight loss. The disadvantages are that it is irreversible, and has a little higher upfront surgical risk. The advantages over gastric bypass are no micronutrient problems and elimination of stomach ulcers and small bowel obstruction.
We Can Help With Your Weight Loss Journey!
What is life like with a Gastric Sleeve?
The weight loss occurs in approximately 12 months. Initially the surgery is very restrictive, but over the next 12mths as the new stomach recovers patients move towards the ability to eat 3 small meals. Post operatively patients are on puree diet for 3 weeks and then progress to a soft diet. By 6mths most people can eat approximately 25% of their previous meals and are able to include all food groups. When going to a restaurant they can eat an entrée sized meal and feel satisfied.
The key point being that a small meal satisfies hence the experience is different to dieting and therefore sustainable in the long term. The early phase is characterized by very early fullness and lack of hunger, which helps with weight loss. But to maintain health there should be a focus on drinking 1liter water per day, 1 multivitamin per day and approx 60 grams of protein per day. Apart from a commitment to “healthy eating” no foods are specifically banned.
After the surgery
DAY ONE: The Day of your operation. When you wake up there will be a “patient controlled analgesic” pump connected to your IV. The nurses will show you the button that releases the medication into your system. This works very well for pain control. You will be asked to sit up and dangle your legs over the edge of the bed four (4) hours after the operation. Your nurse will assist you but you will be required to move yourself. You can have ice to suck to keep your mouth moist.
DAY TWO: The Day after your operation You will be instructed how to use the “incentive spirometer‟. This device is very important. Using it helps your lungs open back up and prevent fluid accumulating. Please use it at least five times an hour while awake. Each time you use it, repeat 10 times. Remember to inhale, raising the balls, hold them there for a second, then exhale. Wait a few seconds, and then repeat. Move your feet and exercise your calf muscles as often as possible. You will also have white stockings (TED) and heparin injections to prevent clots in the leg veins. Your will start a clear fluids diet today. This diet includes clear soup, jelly, juice and cordial. Remember you are not expected to eat all the items on your tray. Take VERY SMALL SIPS, start with a teaspoon and STOP WHEN YOU FULL. Walk as much as possible today.

DAY THREE: Today is the day for you to stabilise and regain your strength. Continue to use your breathing apparatus. You will progress to full fluid diet today. This diet includes soup, yoghurt, custard, milk and cordial. Remember you are not expected to eat all the items on your tray. Take VERY SMALL SIPS, start with a teaspoon and STOP WHEN YOU FULL. If you tolerate the liquid for breakfast, your IV may be removed. All your medications can be taken
by mouth but all tablets need to be crushed. Walk as much as possible today.
DAY FOUR: You may be ready to be discharged on this day or the following day. Your diet will progress to a puree diet. You may eat anything that can be blended. You should eat very slowly. When you sense fullness, STOP. YOU SHOULD AVOID LARGE PARTICLES. On your discharged stay on the same quality of food that you have been on in the hospital. REMEMBER TO TAKE SMALL BITES, CHEW, CHEW, CHEW, AND PUT YOUR FORK/SPOON
DOWN BETWEEN BITES. AT HOME: It is important to maintain an active life. You will do better and reduce your risk of complications if you are working towards getting back to normal quickly. Try to walk at least 5 blocks each and every day. Remember, you are losing weight. You weigh less today than yesterday. Accept that and walk further because you know it’s easier. No other exercises are encouraged at this time. Please do not drive for the first
week. Remember to drink a lot of fluids but avoid soft drinks. Aim for at least 1 liter of water per day. Listen to your “New Stomach”. When you feel full, STOP. Meals should take up to one (30 minutes to 1) hour to complete.
Medications
When you leave hospital you will have prescriptions for medications to be taken after discharge. They include: Somac – This helps to reduce the secretions in the stomach. You should take this for at least 3 months. Analgesia – You will be prescribed specific pain medication. Please take it according to the instructions. . Resume the medications you were taking before surgery except if advised otherwise. Regular checks with your GP or endocrinologist are essential to re-stabilize diabetes and blood pressure medication. NB: All large pills taken during the first six weeks after your operation must be crushed so when you have these prescriptions filled, please purchase a pill crusher.
Expected Post-op Symptoms
DIZZINESS
Occasionally you may feel light headed. This is due to the fact that you are not
drinking as much liquid as you were able to before surgery; therefore the volume in your body is reduced. When this occurs, do not panic. If you can find a comfortable place to sit or lie down, do so. Your body will adjust and the blood will be redistributed adequately after a short interval. However, if this is occurring too frequently, (more than three times a day) please call us. Aim to drink 1.5 liters of fluid per day and monitor your intake. Remember to sip on fluids in between meals and do not worry if you are not drinking a lot of water because juice, milk, soup etc., are all okay.
ALTERED BOWEL HABITS
Bowel habits may be altered after the surgery. In the beginning, you may have watery bowel movements. Do not expect your bowel movements to be regular until you start eating solid food. For most, bowel habits should become regular and you should have one bowel movement every day and usually less in quantity than you are used to. Laxatives can be used such as agarol, lactulose and benefibre.
VOMITING
During the first two months after surgery, you will probably experience a few episodes of vomiting. It is important to remember your new stomach is approximately 100ml and can be easily overwhelmed. You must eat slowly and stop when you feel full. Meals will take up to 45 minutes. Vomiting can occur due to too fast eating, poor chewing and inappropriate food. Follow the dietary advice strictly. Too much vomiting or retching will cause secondary
swelling and possible obstruction of the passageway. If you vomit more than three times a day, call the office. If you cannot keep anything down for more than eight hours, call the office.
NAUSEA
Nausea is a side effect of any gastric operation. This problem may start on the third day after the operation or a couple of weeks after discharge from the hospital. This is the side effect of the operation that is responsible for some of the massive rapid weight loss. Even though you may experience severe nausea you should make an effort to eat at least three or four small meals a day and drink at least three to four cups of water a day. Place one litre of water in the fridge in the morning so you know how much you have drunk during the day. The feeling of nausea may be severe but it is rarely associated with vomiting but if vomiting does occur what comes up is not what was eaten but rather white saliva. If you are vomiting food however, this may need further investigation by X-ray or endoscopic exam.
ANOREXIA
Anorexia, complete lack of appetite, forgetting to eat, is a problem some patients experience. Make an effort to eat at least three to four meals a day.